Introduction
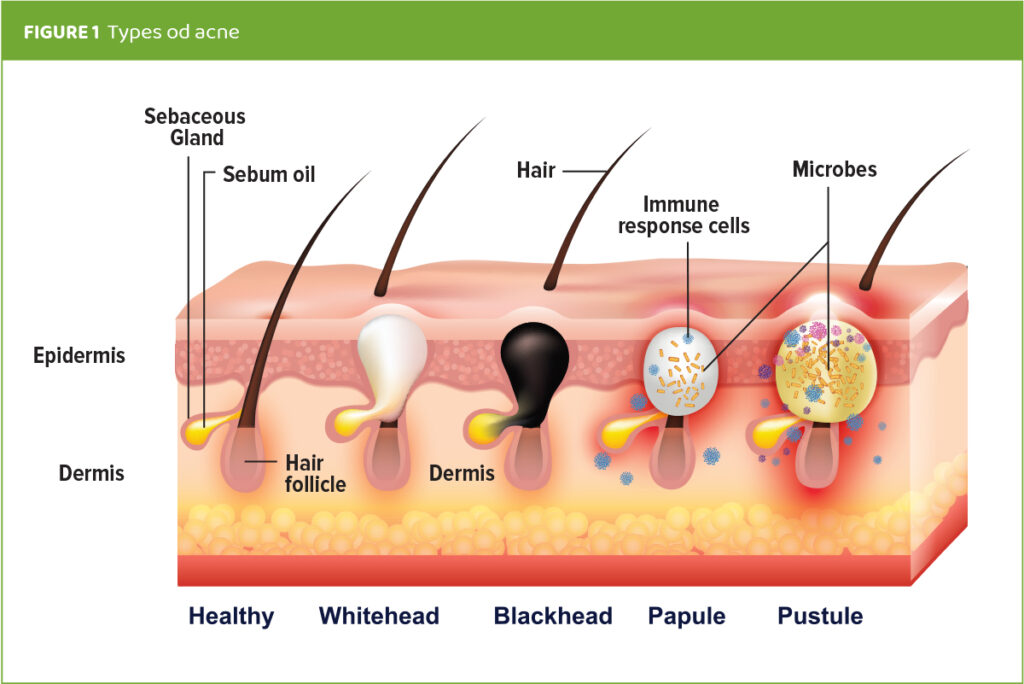
Acne, also known as Acne vulgaris, is a skin condition that occurs when hair follicles become clogged by dead skin cells and excessive sebum, an oily substance secreted by the sebaceous glands that may cause inflammation and dysbiosis of the microbial community. This can result in blackheads or whiteheads, pimples, papules, pustules, oily skin, inflammation, and possible scarring.1,2 (Figure 1) Acne is the eighth most common skin disease in the world according to Heng et al,3 and is an immune-mediated, inflammatory and sometimes chronic condition.4 Primary causes of acne can include genetic predisposition,5 and dysfunction in skin metabolism resulting in increased sebum production.6 Other factors contributing to the prevalence of acne in the general population include hormonal changes, bacterial, yeast, or fungal skin infections, stress, diet, and lifestyle.7
Nigella sativa (N. sativa, family Ranunculaceae), is an annual flowering plant native to southeastern Europe, western Asia, the Middle East, and northern Africa. Oil from its small black seeds, black seed oil (BSO), has been used for centuries as both medicinal and beauty treatments. Black seed oil has been studied more recently for its many health, anti-inflammatory, antioxidant, antifungal, and dermatologic benefits.8-12 Identification of N. sativa’s primary constituent, thymoquinone (TQ), has resulted in a growing interest in its powerful and wide-ranging pharmacological activities.11-17
To harness the incredible power of thymoquinone, TriNutra™ Ltd., has cultivated a full-spectrum, cold-pressed BSO standardized to 3% thymoquinone and very low free fatty acids (FFAs), the highest quality and most powerful thymoquinone concentration available on the market.
Nigella sativa seed oil produced by TriNutra™ Ltd., is a stable, cold-pressed, standardized black seed oil with 3% thymoquinone, the powerful primary active constituent, and a low percentage (<2%) of free fatty acids. This specific formulation is branded as B’utyQuin™ and is a uniquely powerful cosmetic active ingredient. B’utyQuin™ optimizes mitochondrial functions including fat metabolism, ATP production and cell respiration, balances the inflammatory response, and has antioxidant and antimicrobial benefits. It has been shown to target several key mechanisms associated with acne and other cosmetic and dermatologic conditions. This current study’s summary demonstrates the influence of B’utyQuin™ versus Non-Standardized Black Seed Oil (NS-BSO), containing less than 1% thymoquinone and high (+9%) FFAs, on multiple causes associated with acne occurrence, in particular overgrowth of microorganisms.
Mechanisms behind B’utyQuin’s effect on acne occurrence
The black seed oil composition of TriNutra’s B’utyQuin featuring a high thymoquinone content along with low free fatty acids, has been shown to beneficially impact several key modulators of acne. In vitro studies were conducted to determine the mechanisms of action behind BSO’s remarkable benefits for acne. Results highlight the power of thymoquinone’s antimicrobial activity against Propionibacterium (Cutibacterium) acnes (Figure 2), Malassezia furfur, Malassezia globosa, Candida albicans, and Staphylococcus aureus, opportunistic pathogens associated with acne, seborrhea, dandruff and other dermatological conditions.7
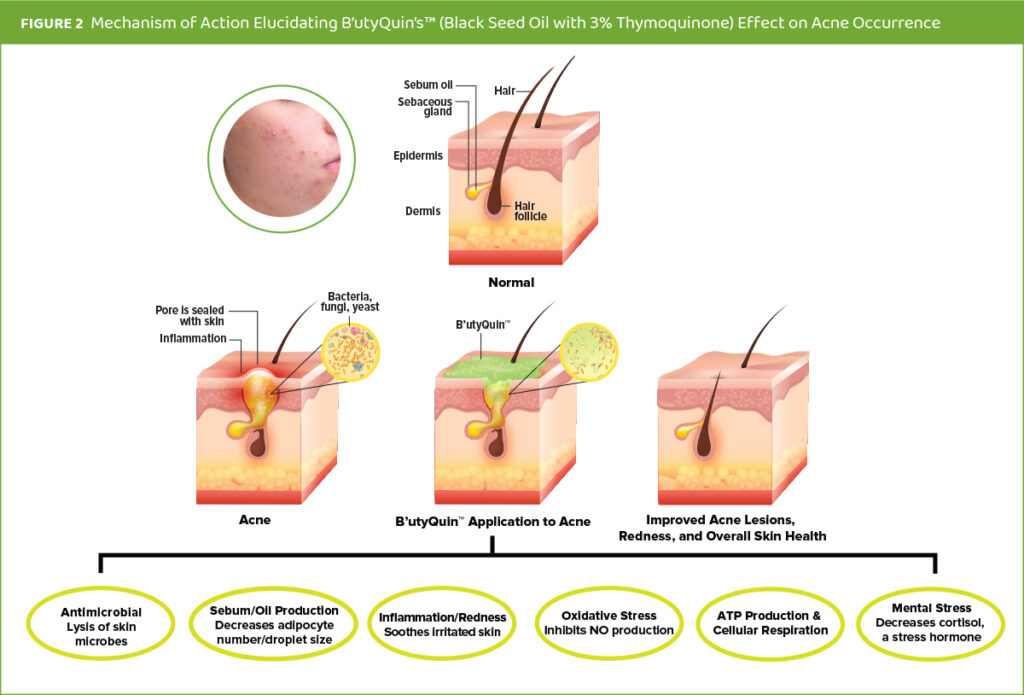
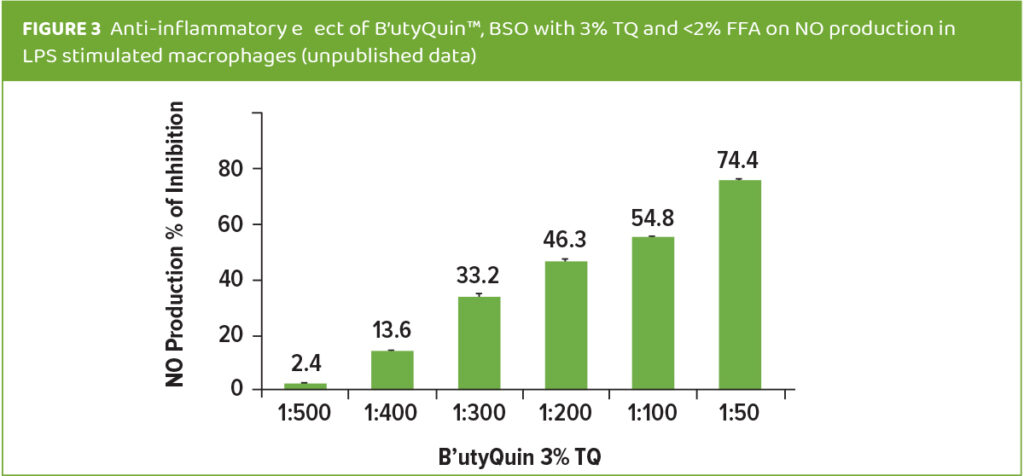
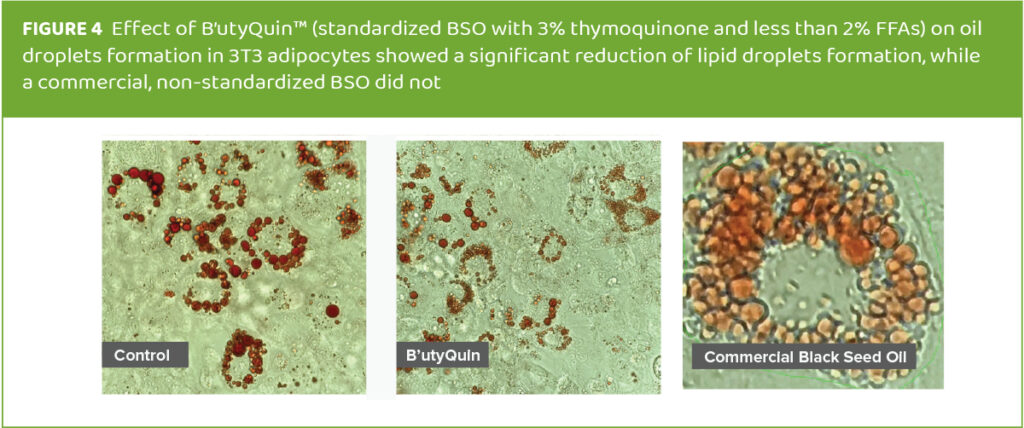
Thymoquinone’s anti-inflammatory properties, via inhibition of nitric oxide production (Figure 3),11 its modulation of fat/sebum metabolism via reduction of adipocyte number and lipid particle size (Figure 4),12 and its immune-modulating properties may help mitigate the inflammatory responses that occur during acne outbreaks. Thymoquinone also modulates sebum production6 which the microorganisms causing acne use for nourishment. Additionally, B’utyQuin’s active ingredient, thymoquinone, can soothe redness, as well as calm and restore harmony to sensitive skin.15,16 Emotional and mental stress are often a contributing factor to acne outbreaks and thymoquinone has been shown to beneficially impact stress, via modulation of the stress hormone, cortisol, when consumed orally.17
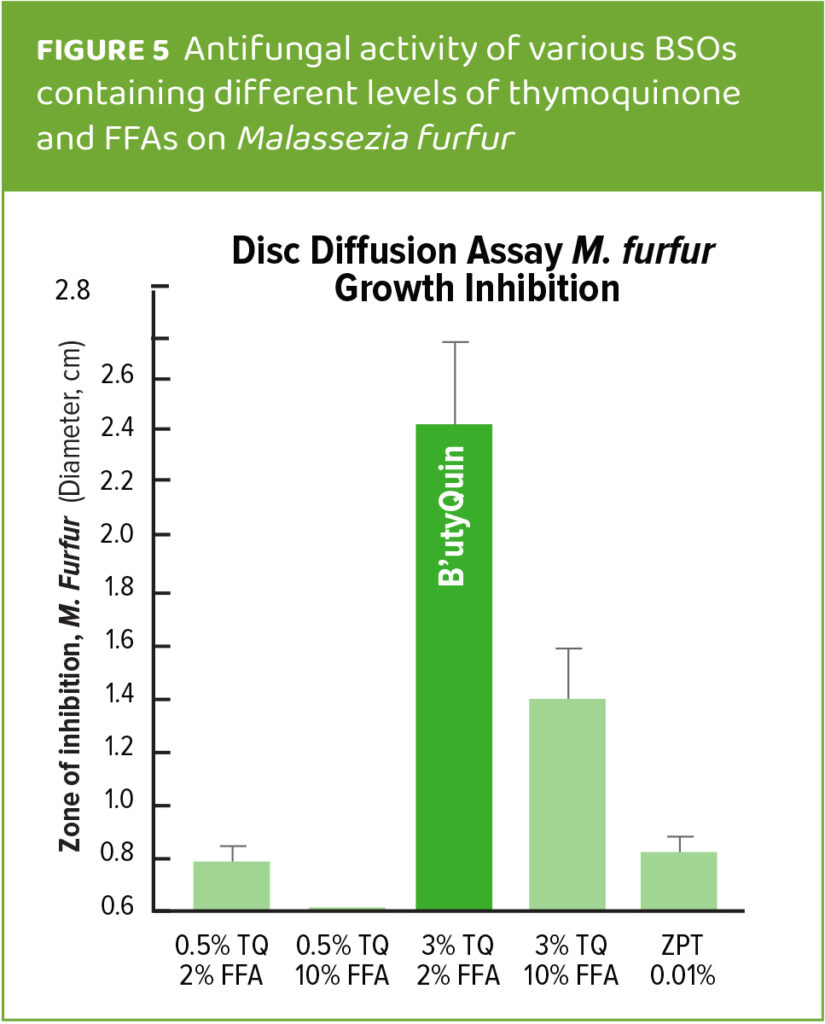
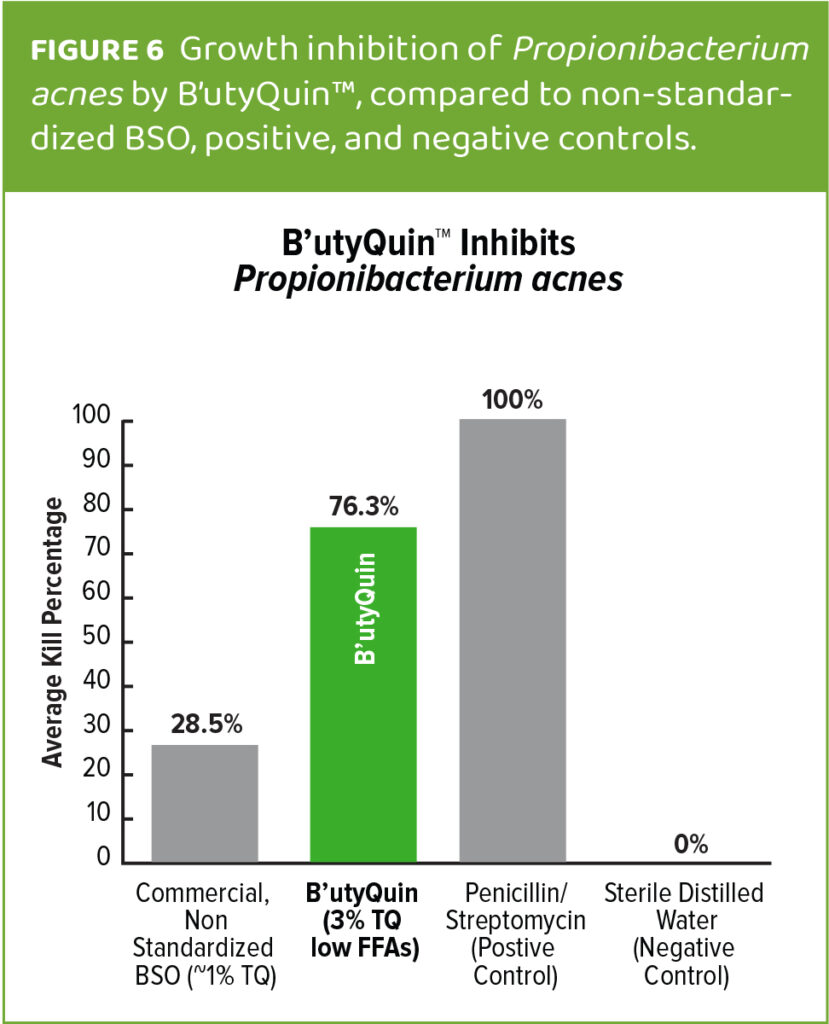
Previous studies have demonstrated B’utyQuin’s antimicrobial activity against Malassezia furfur, (Figure 5) an opportunistic pathogen associated with seborrhea and other dermatological conditions including acne.10 In this study we focus on its ability to significantly inhibit many of the opportunistic pathogens, in particular Propionibacterium acnes, (Figure 6) commonly associated with acne and oily skin in a superior fashion to non-standardized black seed oil. The current study also demonstrates the superiority of B’utyQuin over a non-standardized black seed oil in modulating the microbial diversity present in acne-prone skin.
The following study investigates and compares the influence of standardized black seed oil (B’utyQuin™) and Non-Standardized Black Seed Oil (NS BSO), which contains less thymoquinone and much higher levels of FFAs, on the diversity of microorganisms present on oily skin and often observed with acne.
Organism selection
For this study, the organisms Corynebacterium simulans, Malassezia globosa, Propionibacterium acnes, Staphylococcus capitis, Staphylococcus epidermidis, Staphylococcus hominis and Streptococcus mitis (Table 1) were selected based on their properties related to skin health. The seven test microorganisms used in this study are strains predominantly found on oily skin.18-27

Preparation of B’utyQuin™ and non-standardized black seed oil solutions
A 5% solution of each product was prepared in squalane under sterile conditions with the constituent profiles below:
– B’utyQuin™ – Nigella sativa Seed Oil, by TriNutra, is a stable cold-pressed black seed oil with 3% thymoquinone and less than 2% FFAs
– Non-Standardized Black Seed Oil – from Nigella sativa seeds, containing 0.45% thymoquinone and 9.3% FFAs
– Control – containing 500 µl of phosphate-buffered saline (PBS).
Primary outcome goals
The primary goal of this study was to evaluate the influence of standardized B’utyQuin BSO versus a NS-BSO material on the diversity of the key microorganisms present on oily skin and with acne. The evaluation was conducted to determine whether the standardized black seed oil material (B’utyQuin) had selective and/or stronger antimicrobial efects than the non-standardized material on organisms commonly found on acne prone oily skin.
Study results
Influence of B’utyQuin on the diversity of the key microbes of oily skin
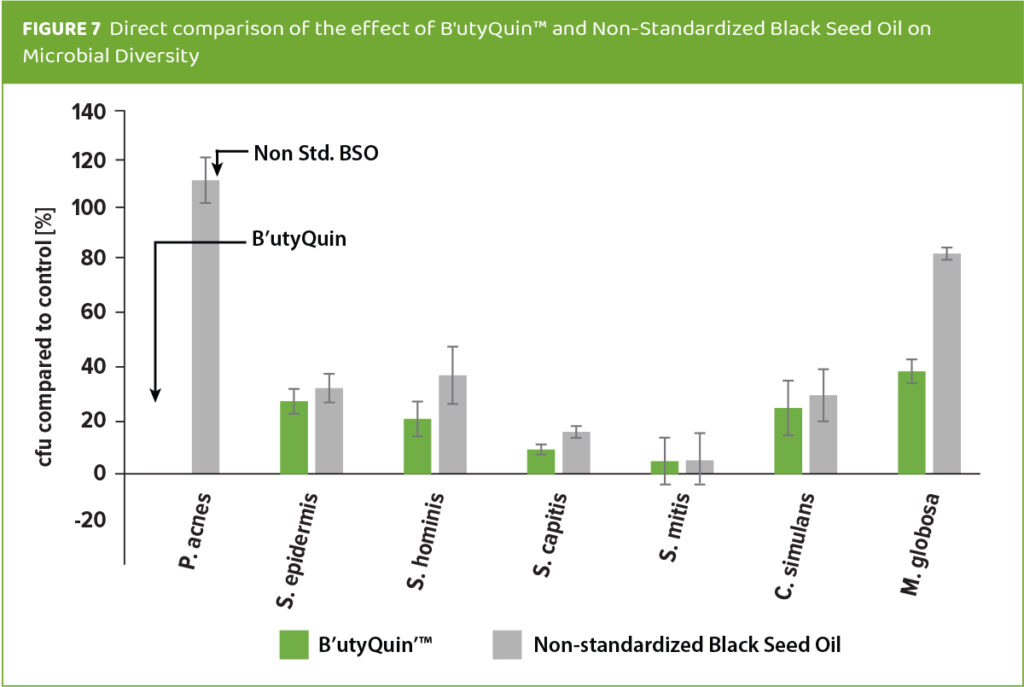
In a co-culture of seven diferent microbial species incubated with a 5% solution of B’utyQuin™ or NS-BSO in squalane for four hours, B’utyQuin demonstrated a selective effect on the microorganism’s diversity. P. acnes was most sensitive to B’utyQuin, as it was completely absent in the diversity culture at the end of the incubation period, while NS-BSO has no inhibitory effect on it. In fact, the growth of P. acnes was enhanced to 108% of the original culture count in the presence of the NS-BSO (Figure 5). This result lends support to an earlier analysis in which B’utyQuin inhibited P. acnes by 76%, as shown in a zone-of-inhibition study on plated agar, compared to NS-BSO or an antibiotic control (Figure 6).
S. mitis was found to be very sensitive to both B’utyQuin and NS-BSO, as only about 5% of the original bacterial count remained at the end of the incubation period with either material.
The Staphylococcus organisms reacted strain specifically to the B’utyQuin and NS-BSO materials. S. epidermidis was the bacterial strain most resistant to incubation with B’utyQuin as demonstrated by -25% of the original bacterial count remaining. However, no statistically significant difference in the growth inhibition of S. epidermidis, S. capitis, S. hominis, S. mitis was observed between the B’utyQuin and NS-BSO materials.
C. simulans incubation with the two materials yielded similar results to S. epidermidis. In total, all bacterial species showed significantly reduced bacterial counts after four hours of incubation with B’utyQuin. The lowest effect of B’utyQuin (yet still significantly inhibitory) was observed for the fungal species, Malassezia globosa, which was inhibited by more than 60% when measured against the starting bacterial culture count. This compares to less than 20% inhibition when incubated with the NS-BSO. (Figure 7). In a separate study, B’utyQuin was also very effective against another Malassezia species, M. furfur, an opportunistic pathogen found on oily skin and acne lesions. (Figure 5.)10
Discussion and conclusion
In the current study, standardized Black Seed Oil with 3% thymoquinone and low content (<2%) of free fatty acids (B’utyQuin™), was analyzed to determine its effect on the diversity of microorganisms commonly found in those with oily skin and/or acne. The results were compared to a Non-Standardized Black Seed Oil (NS-BSO) that contains low amounts of thymoquinone (0.5%) and higher amounts of free fatty acids (9%). The different concentration of the active thymoquinone, between the two materials was postulated to influence its effectiveness on microbial diversity.
For this purpose, using a co-culture of seven organisms, incubated with B’utyQuin™, NS-BSO, or phosphate-buffered saline (PBS) control, the effect on microbial growth was measured and calculated in percentage.
B’utyQuin™ demonstrated a complete inhibitory effect on P. acnes (100%), which was no longer detectable in the culture after the incubation period. Conversely, NS-BSO actually enhanced the growth of P. acnes to 108%, when compared to the control. A similar effect was noticed in a separate Zone of inhibition study of P. acnes comparing B’utyQuin and NS-BSO and an antibiotic.
A strong inhibitory effect on S. mitis was observed for both materials, with only about 5% of the original bacterial count being present after incubation. No statistically significant different effect between the BSO materials was observed in regard to growth rates of S. capitis, S. epidermidis, S. hominis, and C. simulans strains. While the two materials showed the weakest effect on Malassezia globosa, B’utyQuin™ still reduced M. globosa growth by more than 60%, compared to just 19% for the NS-BSO. B’utyQuin’s inhibitory effect on Malassezia globosa is similar to its effect on another opportunistic Malassezia species found on oily skin, Malassezia furfur.
In summary, these results indicate that the standardized Black Seed Oil (B’utyQuin™) has a significantly stronger effect on the microbial growth of microorganisms associated with oily skin and acne than the non-standardized version of black seed oil. The observed strong inhibitory effect is likely attributed to B’utyQuin’s unique standardized composition of its powerful primary constituent, 3% thymoquinone, with a low free fatty acid content. This composition affects sebum/fat production which is a primary source of food for these microorganisms. Other benefits of the standardized BSO and its key active component, thymoquinone such as anti-inflammatory properties,11 modulation of fat/sebum6 as a result of mitochondrial functions boost, reduce skin oiliness and subsequent acne occurrences.15
Thymoquinone may also facilitate increased oxygen and nutrient supply to tissue surfaces via improvement of mitochondrial functions, enhance surface tissue metabolism and turnover, restore and tighten the skin barrier and increase the skin’s resistance to opportunistic pathogens. Additionally, B’utyQuin™ has been shown to soothe redness, calm and restore harmony to sensitive skin.11 Stress is often a contributing factor to acne outbreaks and thymoquinone has been shown to significantly impact stress via modulation of cortisol, the stress hormone, when consumed orally.17
This study and previous research highlight the superiority of a standardized BSO (B’utyQuin™ with 3% thymoquinone and <2% FFA) over non-standardized BSO in mitigating several of the key factors involved in acne occurrence as illustrated in Figure 2.
About TriNutra®:
TriNutra® was born from the ownership group’s vision to serve unmet needs with formulations possessing immediate action and efficacy. The TriNutra® difference and approach to product development is based on three scientific concepts:
• A synergistic combination of ingredients in a proper ratio for optimal efficacy
• The proper therapeutic dosage of each ingredient
• Clinical research to support the efficacy of the combination of product ingredients.
• TriNutra® appreciates your interest in TriNutra® and looks forward to supporting your practice with innovative, efficacious, and clinically validated formulations.
References:
1 Williams HC, Dellavalle RP, Garner S. The Lancet. 2012; 379 (9813):361-372. doi.org/10.1016/s0140- 6736(11)60321-8.
2 Mahto A. Medicine. 2017;45(6):386–389.doi.org/10.1016/j.mpmed.2017.03.003.
3 Heng AH, Chew FT. Sci Rep. 2020;10(1):5754. doi: 10.1038/ s41598-020-62715-3.
4 The Institute for Health Metrics and Evaluation (IHME). GBD 2019. https://www.healthdata.org/research-article/global-burde-ch ronic-respiratory-diseases-and-risk-factors-1990–2019-upda te-global. Accessed Aug 12, 2023.
5 Ballanger F, Baudry P, N’Guyen JM, et al. Dermatology. 2006;212(2):145–149. doi:10.1159/000090655
6 Zouboulis CC, Jourdan E, Picardo M. J Eur Acad Dermatol Venereol. 2014;28(5):527–532. doi: 10.1111/jdv.12298.
7 Heng AH, Say YH, Sio YY, et al. Dermatology. 2022;238(2):226-235. doi:10.1159/000516232.
8 Matthaus B, Özcan MM. Czech J Food Sci. 2011;29(2):145-150. No doi.
9 Cheikh-Rouhou S, Besbes S, Hentati B, et al. Food Chemistry. 2007;101(2):673-681. No doi.
10 Ogen-Shtern N, Margarita Y, von Oppen-Bezalel L. Food Sci Nutr Res. 2021;4(2):1-9. No doi.
11 Yeun K, Akshay A, Raffaelle M, et al. J Food Nutr Sci. 2021;3(3):63-74. No doi.
12 Shen HH, Peterson SJ, Bellner L, et al. Antioxidants (Basel). 2020;9(6):489. doi: 10.3390/antiox9060489
13 Unpublished Research by TriNutra™ on ThymoQuin™ Synergies. 2018. Pharmaseed, Nes Ziona Israel.
14 Licari M, Raffaelle M, Rosman ZF, et al. J Nutr Food Sci. 2019;9:751. doi:10.4172/2155-9600.1000751.
15 von Oppen-Bezalel L, Jurenka JS. SOFW7Days. 2022;147:1-7. No doi.
16 Al Ghamdi MS. J Ethnopharmacol. 2001;76(1):45-48. doi: 10.1016/s0378-8741(01)00216-1.
17 Talbott SM, Talbott JA. EC Nutrition. 2022;17(7):18-27. No doi.
18 Ridaura VK, Bouladoux N, Claesen J, et al. J Exp Med. 2018;215(3):785-799. doi: 10.1084/jem.20171079.
19 Wattiau P, Janssens M, Wauters G. Int J Syst Evol Microbiol. 2000;50(Pt 1):347-353. doi: 10.1099/00207713-50-1-347.
20 Saxena R, Mittal P, Clavaud C, et al. Front Cell Infect Microbiol. 2018 Oct 4;8:346. doi: 10.3389/fcimb.2018.00346.
21 Saxena R, Mittal P, Clavaud C, et al. Sci Rep.2021;11(1):7220. doi: 10.1038/s41598-021-86454-1.
22 Gilchrist TC. Johns Hopkins Hospital Report 1900;9:409-430. No doi.
23 Dekio I, McDowell A, Sakamoto M, et al. Int J Syst Evol Microbiol. 2019;69(4):1087-1092. doi: 10.1099/ijsem.0.003274.
24 Heath V, Cloutman-Green E, Watkin S, et al. Antibiotics (Basel). 2023;12(4):669. doi: 10.3390/antibiotics12040669.
25 Winslow CE, Winslow AR. 1908. The Systematic Relationships of the Coccaceae. New York. pp. 1-300. John Wiley and Sons.
26 Severn MM, Williams MR, Shahbandi A, mBio. 2022;13(3):e0093022. doi: 10.1128/mbio.00930-22.
27 Wei Y, Joyce LR, Wall AM, et al. mSphere. 2021;6(1):e01099-20. doi: 10.1128/mSphere.01099-20.




