AUTHOR: Sara Kralj, MSc, Master in Nutrition
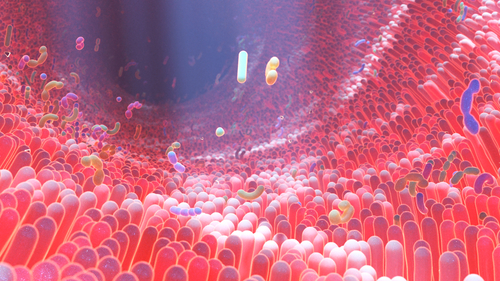
The gut-endocrine system represents a key link between diet, metabolism, and the microbiota. Enteroendocrine L-cells of the gut respond to the presence of nutrients and microbial metabolites by secreting hormones that influence glucose homeostasis, appetite, and energy metabolism1. Among these hormones, glucagon-like peptides (GLP-1 and GLP-2) play a central role in communication between the gut and other organ systems. These hormones act via specific G-protein-coupled receptors (GLP-1R and GLP-2R), which are differentially distributed across tissues, determining their physiological function2.
GLP-1 – role in metabolic regulation
Glucagon-like peptide-1 (GLP-1) is a 30-amino-acid hormone secreted from enteroendocrine L-cells in response to nutrient intake, especially glucose. Two bioactive forms exist (GLP-1₇₋₃₇ and GLP-1₇₋₃₆ amide), and their secretion is stimulated by dietary components in the proximal gut as well as by microbial metabolites in distal gut regions, such as short-chain fatty acids (SCFAs), indoles, and bile acids3,4. In this way, the microbiota participates in the regulation and prolonged secretion of GLP-1 and peptide YY (PYY) after meals, maintaining postprandial homeostasis1.
GLP-1 exerts multiple metabolic effects. It stimulates insulin synthesis and secretion in pancreatic β-cells while simultaneously inhibiting glucagon secretion, contributing to improved glucose homeostasis. By acting on the gastrointestinal tract, it slows gastric emptying and reduces gastric acid secretion, thereby lowering postprandial glycemia and enhancing satiety1,5.
GLP-1 actions are mediated through specific GLP-1 receptors (GLP-1R) located in the pancreas, central nervous system (hypothalamus, brainstem, mesolimbic system), and peripheral tissues such as muscle and adipose tissue. Activation of GLP-1R in the brain reduces appetite, while in muscle and adipose tissue, GLP-1R agonists promote glucose uptake via AMP-activated protein kinase (AMPK) activation and GLUT-4 translocation, mimicking insulin effects. GLP-1R agonists (e.g., exenatide, liraglutide) also exert cytoprotective effects, promoting proliferation and reducing apoptosis of pancreatic β-cells, thereby preserving their function and improving insulin sensitivity1.
Endogenous GLP-1 is rapidly degraded by dipeptidyl peptidase-4 (DPP-4), but part of its effect is mediated via vagal afferent nerves. Vagus nerve activation (n. vagus) is critical for GLP-1’s anorectic and incretin effects, as vagotomy abolishes GLP-1-induced appetite suppression. This connection, known as the neuroendocrine-incretin effect, links peripheral and central GLP-1 actions in regulating food intake and glucose metabolism1,6.
In conclusion, GLP-1 represents a central regulator of glycemic control and appetite, with its actions arising from a complex interplay between the gut, microbiota, endocrine cells, and nervous system.
GLP-2 – role in maintaining gut integrity
GLP-2, secreted concurrently with GLP-1 in approximately equal ratios, acts primarily locally in the gut via GLP-2 receptors (GLP-2R). Its main functions include stimulating crypt cell proliferation, promoting intestinal mucosal growth, and epithelial regeneration7,8,9,10,11. Through these effects, GLP-2 contributes to the maintenance of gut barrier integrity and reduced intestinal permeability, indirectly supporting systemic metabolic balance and immune homeostasis2.
Impact of the gut microbiota on GLP-1
The gut microbiota significantly influences the secretion and activity of GLP-1. Microbial metabolites such as short-chain fatty acids (SCFAs), indoles, and secondary bile acids stimulate L-cells to secrete GLP-1 while simultaneously improving the sensitivity of target tissues to insulin and insulin signaling. Dysbiosis, defined as an imbalance in the microbiota composition, is associated with altered GLP-1 responses, reduced secretion, and the development of metabolic disorders such as insulin resistance, fatty liver, and obesity1,5.
At the level of the gut barrier, GLP-1 reduces intestinal permeability and bacterial translocation, thereby contributing to gut integrity preservation and reduction of systemic inflammation associated with metabolic disorders. In energy metabolism, GLP-1 promotes lipolysis and energy expenditure, enhances glycogen storage in the liver, and reduces hepatic glucose output. Its effects on the central nervous system manifest as appetite suppression in the hypothalamus and increased satiety, contributing to decreased food intake and body weight regulation5.
Microbial metabolites in GLP-1 secretion control
The secretion of GLP-1 from enteroendocrine L-cells results from a complex network of interactions between dietary components, microbial metabolites, and endocrine signaling. The gut microbiota produces numerous bioactive molecules that directly or indirectly regulate L-cell function, thereby influencing glucose homeostasis, appetite, and body weight5.
Short-chain fatty acids (SCFAs), such as acetate, propionate, and butyrate, are key microbial metabolites generated through the fermentation of indigestible dietary fibers in the colon. Since the human genome encodes fewer than 20 enzymes capable of digesting complex carbohydrates, a significant portion of polysaccharides reaches the colon undigested, where the microbiota degrades them via carbohydrate-active enzymes12. This process results in high SCFA concentrations precisely in gut regions abundant in L-cells, highlighting the physiological significance of this local interaction. Over 90% of SCFAs are absorbed by the intestinal epithelium or further metabolized by the microbiota, while the remainder acts locally on L-cells through free fatty acid receptors GPR43 (FFAR2) and GPR41 (FFAR3)5,13. Activation of these receptors increases intracellular calcium, promoting GLP-1 and peptide YY (PYY) secretion. Notably, reduced SCFA production or fermentation capacity is linked to metabolic diseases, including type 2 diabetes, further underscoring their role in metabolic regulation5,14,15.
Secondary bile acids (BAs) also act as important signaling molecules in GLP-1 regulation. Primary bile acids, cholic acid (CA) and chenodeoxycholic acid (CDCA), synthesized in the liver, undergo microbial conversion into secondary forms – lithocholic acid (LCA) and deoxycholic acid (DCA). Since these transformations depend on bacterial activity, changes in gut microbiota composition can significantly affect the quantity and ratio of secondary BAs. Secondary BAs exhibit dual regulatory effects on GLP-1 secretion: they activate the Takeda G-protein-coupled receptor 5 (TGR5) on L-cell surfaces, stimulating GLP-1 release16,17, but can also exert inhibitory effects via farnesoid X receptor (FXR) activation, reducing hormone synthesis and secretion18,19. This establishes a fine balance between stimulatory and inhibitory signals depending on bile acid type and concentration.
In addition to SCFAs and bile acids, other microbial metabolites modulate GLP-1 secretion. 2-Oleoyl glycerol (2-OG), derived from dietary fat digestion, activates GPR119 receptors on L-cells, while indoles, products of bacterial tryptophan metabolism, also stimulate GLP-1 secretion. Lipopolysaccharides (LPS), components of gram-negative bacterial cell walls, can further activate GLP-1 secretion via Toll-like receptor 4 (TLR4), linking microbial signaling to metabolic and inflammatory processes5.
Overall, these complex mechanisms demonstrate that GLP-1 secretion is closely associated with gut microbiota activity. Metabolites such as SCFAs and secondary bile acids serve as key signaling molecules in the microbiota-host communication, mediating interactions between nutrient intake, microbial fermentation, and endocrine responses. Maintaining a balanced gut microbiota and optimal metabolite production is therefore a fundamental factor in preventing and managing metabolic disorders associated with impaired GLP-1 signaling5.
Impact of prebiotics and probiotics on GLP-1 Secretion
Prebiotics and probiotics play an important role in modulating the gut microbiota and stimulating the secretion of intestinal peptides, including glucagon-like peptide-1 (GLP-1) and peptide YY (PYY). Their effects are based on improving gut barrier integrity, modulating immune responses, and influencing microbial metabolites such as short-chain fatty acids (SCFAs) and bile acids, which directly stimulate enteroendocrine cells5.
Prebiotics
Prebiotics, including oligofructose, fructans, resistant starch, and arabinoxylan-oligosaccharides, are fermented by the gut microbiota, increasing SCFA production (acetate, propionate, and butyrate). These metabolites activate GPR41 and GPR43 receptors on L-cells, promoting the secretion of GLP-1 and PYY5,20.
Although the role of prebiotics in modulating intestinal peptide secretion is well documented in experimental models, clinical results in humans remain inconsistent5. Some studies reported that oligofructose supplementation increased PYY concentration but not GLP-121,22. Conversely, arabinoxylan-oligosaccharide supplementation reduced early postprandial GLP-1 secretion, accompanied by decreased gut microbiota alpha diversity and increased relative abundance of the genera Bifidobacterium, Akkermansia, and Lactobacillus23. In hyperinsulinemic subjects, increased dietary fiber intake stimulated SCFA production, particularly acetate and butyrate, leading to elevated plasma GLP-1 levels and higher fasting and postprandial insulin concentrations, although without significant changes in body weight24. Furthermore, a low-carbohydrate almond-based diet significantly increased the relative abundance of Roseburia and Ruminococcus, known SCFA producers, along with increased GLP-1 concentrations25,26. Overall, clinical prebiotic interventions show heterogeneous effects on GLP-1 secretion, indicating the need for further standardized research to clarify their specific mechanisms and interindividual response variability.
Animal studies highlight significant variability in prebiotic effects on GLP-1 secretion. In animal models, prebiotics promoted the growth of butyrate-producing bacteria27, increased GLP-1 secretion, and improved glucose homeostasis5. For example, Dendrobium polysaccharides increased the abundance of Akkermansia and Parabacteroides, as well as SCFA, tryptophan, and indole concentrations, stimulating GLP-1 secretion28. Similarly, resveratrol and tetrahydrocurcumin enhanced GLP-1 release alongside changes in microbiota composition29,30. Prebiotics such as oligofructose, fructo-oligosaccharides, fructans, and inulin increased GLP-1, PYY, and SCFA levels, although microbiota structural changes were not always consistent5. In type 2 diabetes models, fiber supplementation increased the abundance of Akkermansia muciniphila and Bacteroidetes, decreased Firmicutes and Proteobacteria, resulting in higher GLP-1 levels and improved metabolic parameters31.Additionally, flavonoids from Lycium barbarum and polysaccharides from adlay seeds modulated the microbiota and inflammatory processes while increasing GLP-1 and producing hypoglycemic effects32,33. Overall, prebiotics can beneficially affect GLP-1 secretion via gut microbiota modulation and enhanced SCFA production.
Probiotics
Probiotics also show potential in modulating GLP-1 secretion through changes in gut microbiota composition and activity. Supplementation with Anaerobutyricum soehngenii increased secondary bile acids and postprandial GLP-1, improving glucose metabolism34. Administration of Lactobacillus reuteri increased GLP-1 and insulin secretion in individuals with impaired glucose tolerance, while the probiotic mixture VSL#3 (containing eight strains including Streptococcus thermophilus, Bifidobacterium [B. breve, B. infantis, B. longum], Lactobacillus acidophilus, L. plantarum, L. paracasei, and L. delbrueckii subsp. bulgaricus)elevated GLP-1 levels and reduced BMI in children with non-alcoholic fatty liver disease over four months35,36.
A study in type 2 diabetic mice consuming Kombucha (a source of polyphenols and organic acids) showed improved inflammation and gut barrier integrity, with reduced LPS levels and increased expression of zonula occludens-1, claudin-1, occludin, and mucin. Simultaneously, SCFA-producing bacterial abundance increased, resulting in higher SCFA levels and elevated GLP-1 and PYY concentrations37. Exopolysaccharides from Bacillus amyloliquefaciens also increased GLP-1 levels through gut tissue interaction38. VSL#3 supplementation for eight weeks increased butyrate-producing bacteria, butyrate levels, and GLP-1, improving glucose tolerance in diabetic and obese mice39.
A recombinant Lactobacillus paracasei NFBC 338 strain expressing a long-acting GLP-1 analog improved glucose and lipid metabolism in diet-induced obese rats without significant cecal microbiota changes40. Similarly, composite probiotic supplementation enhanced GLP-1 and PYY secretion via microbiota modulation and increased SCFA production, improving glucose and lipid metabolism and pancreatic function in diabetic mice41. Oral administration of Lactobacillus casei increased the abundance of Bacteroidetes, Bifidobacterium, and Lactobacillus, resulting in enhanced butyrate production and GLP-1stimulation42. Clostridium butyricum CGMCC0313.1 reduced the Firmicutes/Bacteroidetes ratio, increased SCFA-producing bacteria and FFAR2/FFAR3 receptor expression, and raised GLP-1 levels in serum and ileum, although this effect was absent in db/db mice with leptin receptor defects43. Supplementation with L. fermentum MCC2759/MCC2760 reduced pathogenic bacteria, increased Lactobacillus spp., and promoted GLP-1 production44,45. Furthermore, L. rhamnosus LGG increased beneficial bacterial abundance and GLP-1 levels, with elevated acetate and propionate concentrations46. In piglets, L. plantarum supplementation decreased Bacteroides and Parabacteroides abundance and lithocholic acid (LCA) levels, resulting in improved glucose metabolism47.
Impact of the gut microbiota on GLP-1 function
Incretin-based drugs have proven highly effective in treating type 2 diabetes. Numerous studies indicate that the incretin effect is impaired in individuals with obesity, impaired glucose tolerance (IGT), and type 2 diabetes. However, in some cases, reduced therapeutic efficacy of GLP-1 receptor agonists (GLP-1 RA) occurs, leading to treatment discontinuation. This phenomenon, known as GLP-1 resistance, may be associated with gut microbiota dysbiosis5.
Clinical research shows that gut microbiota composition can influence the efficacy of GLP-1 receptor agonist therapy. In a study of patients receiving liraglutide or dulaglutide, only a subset exhibited reductions in HbA1c and BMI. Microbiota analysis revealed significant differences in beta diversity between these groups, including the presence of bacterial species such as Bacteroides dorei and Roseburia inulinivorans, suggesting that microbiota profiles may predicttherapeutic response5,48.
Experimental models further confirm the link between dysbiosis and GLP-1 resistance. A 2017 study developed two mouse models of type 2 diabetes – diabetic obesity and diabetic leanness. Following an oral glucose tolerance test (OGTT), glucose levels were similar across groups, but lean diabetic mice had higher plasma GLP-1 concentrations and lower insulin levels, indicating the development of GLP-1 resistance. Transplantation of the ileal microbiota from these mice into germ-free animals resulted in impaired incretin response, confirming that GLP-1 function depends on gut microbiota balance. Dysbiosis can therefore directly weaken the GLP-1 response48,49.
Impact of the gut microbiota on the circadian rhythm of GLP-1 secretion
Circadian rhythms are endogenous, approximately 24-hour cycles that regulate numerous physiological processes in the body, including metabolism and hormone secretion. In addition to the central nervous system, the biological clock is present in peripheral tissues such as the pancreas and gastrointestinal tract, where genes like CLOCK and BMAL1 coordinate metabolic functions50,51. Dysfunction of these genes has been associated with the development of metabolic disorders, including diabetes mellitus5.
GLP-1 secretion also follows a circadian pattern. Studies in humans and animal models have shown that GLP-1 secretion is higher in the morning, while the lowest levels are observed in the evening or early morning hours52. These oscillations reflect the rhythmic activity of intestinal L cells, whose GLP-1 release depends on the expression of clock genes, particularly BMAL1, PER1/2/3, DBP, and TEF5.
The gut microbiota plays a key role in regulating the circadian rhythm of GLP-1 secretion. Studies in germ-free mice have shown that the absence of gut bacteria disrupts the rhythmic secretion of insulin and GLP-1, whereas their rhythm is restored after microbiota transplantation from healthy animals53. Furthermore, the biological rhythms of L cells, especially the expression of clock genes such as Bmal1, Per1/2/3, Dbp, and Tef, regulate GLP-1 release. Reduced expression of Bmal1 leads to disturbances in circadian GLP-1 secretion54,55. Therefore, gut microbiota balance and proper L cell function jointly maintain the physiological rhythm of GLP-1 secretion.
Impact of GLP-1 on the gut microbiota
GLP-1 analogs and microbiota modulation
Recent research shows that drugs acting through the incretin system, particularly GLP-1 receptor agonists (GLP-1 RA), can influence the composition and functionality of the gut microbiota, extending beyond their primary pharmacological effects. Liraglutide is an example of a GLP-1 analog that, in experimental animal studies, increases the proportion of short-chain fatty acid (SCFA)-producing bacteria, including Bacteroides and members of the Lachnospiraceae family, as well as probiotic genera such as Bifidobacterium56. Notably, an increase in Akkermansia muciniphila, a bacterium associated with intestinal homeostasis and metabolic health, has been observed57,58,59.
In human studies, liraglutide administration increased microbiota diversity and richness, with a notable rise in the relative abundance of Bacteroidetes, Proteobacteria, and Bacilli60. However, results have not always been consistent. Combined therapy with metformin or sulfonylureas sometimes masked the effects of liraglutide on the microbiota, while in older populations with type 2 diabetes, no significant changes in gut microbiota diversity were observed61. Additionally, liraglutide may act via activation of the gut sympathetic nervous system, representing an alternative mechanism for microbiota modulation62. Overall, GLP-1 analogs demonstrate the capacity to positively modulate the gut microbiota, although the extent of this effect depends on the therapeutic context and study population5.
DPP-4 inhibitors and microbiota
Dipeptidyl peptidase-4 (DPP-4) inhibitors improve oral glucose tolerance and elevate plasma GLP-1 concentrations, with concomitant changes in gut microbiota composition. Clinical studies using vildagliptin monotherapy in type 2 diabetes patients have shown a reduction in Bacteroidetes abundance89, whereas in animal models, linagliptin and sitagliptin increasedthe proportion of Bacteroidetes and succinate concentration, an important metabolite for energy metabolism63,64.
Vildagliptin additionally reduced Oscillibacter spp. and increased Lactobacillus spp. and propionate levels in animals fed a Western diet65,66. Furthermore, DPP-4 inhibitors, such as PKF-275-055 and vildagliptin, decreased the Firmicutes/Bacteroidetes ratio and increased SCFA-producing bacteria, effects comparable to metformin67,68. Overall, DPP-4 inhibitors moderately correct gut microbiota dysbiosis in obesity and type 2 diabetes.
Bidirectional communication between GLP-1 and the microbiota
Disruption of the gut microbiota can promote endotoxemia and the development of insulin resistance. In type 2 diabetes, there is an increased proportion of gram-negative Enterobacteriaceae and a reduced number of acetate-producing bacteria, such as Bifidobacterium, resulting in elevated LPS release and decreased acetate production69. LPSbinds to Toll-like receptor 4 (TLR4), disrupting the gut barrier69 and increasing serum LPS levels, contributing to inflammation in prediabetes70,71.
As compensation, enteroendocrine cells increase GLP-1 secretion in response to LPS exposure, and the cytokine IL-6 further stimulates its release5,72. GLP-1 promotes insulin synthesis, enhances satiety, and reduces food intake through GLP-1 receptors73, whose agonist, exendin-4, exhibits anti-inflammatory effects by inhibiting cytokine production and macrophage infiltration74. Therapeutic interventions that elevate GLP-1 levels have shown beneficial effects on the intestinal inflammatory response, confirming the immunomodulatory role of this hormone.
Gut hormones as regulators of the microbiota
The gut microbiota operates in symbiosis with enteroendocrine cells (EECs), which are distributed among the epithelial cells of the intestinal mucosa and secrete various hormones. L cells, which produce GLP-1 and PYY, are predominantly located in the distal intestine and colon5. These peptides influence appetite, satiety, and food intake, while changes in the gut microbiota can reciprocally affect eating behavior75,76. Intestinal peptides also regulate gut motility and permeability77 and may possess antimicrobial and protective properties78. For example, peptide D3 increases the abundance of Akkermansia muciniphila and reduces appetite, whereas milk-derived peptides improve gut barrier integrity79. Overall, intestinal peptides serve as key mediators of communication between the gut microbiota and the host.

Conclusion
The interaction between GLP-1 and the gut microbiota represents a complex bidirectional system that regulates host metabolism, appetite, and immune responses. The gut microbiota, through the production of metabolites such as short-chain fatty acids (SCFAs), indoles, and secondary bile acids, stimulates GLP-1 secretion, while GLP-1 modulates gut microbiota function and metabolic responses in the brain, intestines, and pancreas. Interventions such as prebiotics, probiotics, GLP-1 analogs, DPP-4 inhibitors, or bariatric surgery alter microbiota composition and activity, improving host metabolism and potentially enhancing therapeutic responses. Although study results remain heterogeneous, evidence suggests that modulation of the gut microbiota can indirectly enhance GLP-1 secretion and the production of key microbial metabolites, opening the way for personalized strategies in the prevention and treatment of metabolic disorders, including obesity and type 2 diabetes. Future application of multi-omic technologies may further clarify these relationships and support individualized therapeutic approaches based on GLP-1 and gut microbiota interactions.
References:
- Longo S, Rizza S, Federici M. Microbiota-gut-brain axis: relationships among the vagus nerve, gut microbiota, obesity, and diabetes. Acta Diabetol. 2023 Aug;60(8):1007-1017.
- Abdalqadir N, Adeli K. GLP-1 and GLP-2 Orchestrate Intestine Integrity, Gut Microbiota, and Immune System Crosstalk. Microorganisms. 2022 Oct 19;10(10):2061.
- Sam AH, Troke RC, Tan TM, Bewick GA. Uloga crijevno-mozdane osi u modulaciji unosa hrane. Neuropharmacology. 2012;63:4656.
- Richards P, Thornberry NA, Pinto S. Os crijeva i mozga: Identificiranje novih terapijskih pristupa za dijabetes tipa 2, pretilost i srodne poremećaje. Mol Metab. 2021;46:101175.
- Zeng Y, Wu Y, Zhang Q, Xiao X. Crosstalk between glucagon-like peptide 1 and gut microbiota in metabolic diseases. mBio. 2024 Jan 16;15(1):e0203223.
- Krieger JP, Arnold M, Pettersen KG, Lossel P, Langhans W, Lee SJ. Smanjenje GLP-1 receptora u vagalnim aferentnim vlaknima utječe na normalan unos hrane i glikemiju. Dijabetes. 2016
- Tsai CH, Hill M., Asa SL, Brubaker PL, Drucker DJ Svojstva glukagonu sličnog peptida-2 koja potiču rast crijeva u miševa. Am. J. Physiol. Endocrinol. Metab. 1997;273:E77–E84. doi: 10.1152/ajpendo.1997.273.1.E77.
- Thulesen J., Hartmann B., Hare KJ, Kissow H., Ørskov C., Holst JJ, Poulsen SS Glukagonu sličan peptid 2 (GLP-2) ubrzava rast neoplazmi debelog crijeva u miševa. Gut. 2004;53:1145– 1150
- Estall JL, Drucker DJ Glukagonu sličan peptid-2. Annu. Rev. Nutr. 2006;26:391–411.
- Brubaker PL Glukagonu sličan peptid-2 i regulacija rasta i funkcije crijeva. Compr. Physiol. 2011;8:1185–1210.
- Chen ME, Naeini SM, Srikrishnaraj A., Drucker DJ, Fesler Z., Brubaker PL Glukagonu sličan peptid-2 stimulira ulazak u S-fazu crijevnih Lgr5+ matičnih stanica. Cell. Mol. Gastroenterol. Hepatol. 2022;13:1829–1842.
- Cantarel BL, Lombard V, Henrissat B. 2012. Complex carbohydrate utilization by the healthy human microbiome. PLoS One 7:e28742.
- Brown AJ, Goldsworthy SM, Barnes AA, Eilert MM, Tcheang L, Daniels D, Muir AI, Wigglesworth MJ, Kinghorn I, Fraser NJ, Pike NB, Strum JC, Steplewski KM, Murdock PR, Holder JC, Marshall FH, Szekeres PG, Wilson S, Ignar DM, Foord SM, Wise A, Dowell SJ. 2003. The orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J Biol Chem 278:11312–11319.
- Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, Nielsen T, Pons N, Levenez F, Yamada T, et al. 2010. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 464:59–65.
- Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, Almeida M, Arumugam M, Batto J-M, Kennedy S, et al. 2013. Richness of human gut microbiome correlates with metabolic markers. Nature 500:541–546.
- Harach T, Pols TWH, Nomura M, Maida A, Watanabe M, Auwerx J, Schoonjans K. 2012. TGR5 potentiates GLP-1 secretion in response to anionic exchange resins. Sci Rep 2:430.
- Thomas C, Gioiello A, Noriega L, Strehle A, Oury J, Rizzo G, Macchiarulo A, Yamamoto H, Mataki C, Pruzanski M, Pellicciari R, Auwerx J, Schoonjans K. 2009. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab 10:167–177.
- Trabelsi MS, Daoudi M, Prawitt J, Ducastel S, Touche V, Sayin SI, Perino A, Brighton CA, Sebti Y, Kluza J, et al. 2015. Farnesoid X receptor inhibits glucagon-like peptide-1 production by enteroendocrine L cells. Nat Commun 6:7629.
- Ducastel S, Touche V, Trabelsi MS, Boulinguiez A, Butruille L, Nawrot M, Peschard S, Chávez-Talavera O, Dorchies E, Vallez E, Annicotte JS, Lancel S, Briand O, Bantubungi K, Caron S, Bindels LB, Delzenne NM, Tailleux A, Staels B, Lestavel S. 2020. The nuclear receptor FXR inhibits glucagon-like peptide-1 secretion in response to microbiota-derived short-chain fatty acids. Sci Rep 10:174.
- Cani PD, Lecourt E, Dewulf EM, Sohet FM, Pachikian BD, Naslain D, De Backer F, Neyrinck AM, Delzenne NM. 2009. Gut microbiota fermentation of prebiotics increases satietogenic and incretin gut peptide production with consequences for appetite sensation and glucose response after a meal. Am J Clin Nutr 90:1236–1243.
- Parnell JA, Reimer RA. 2009. Weight loss during oligofructose supplementation is associated with decreased ghrelin and increased peptide YY in overweight and obese adults. Am J Clin Nutr 89:1751–1759.
- Daud NM, Ismail NA, Thomas EL, Fitzpatrick JA, Bell JD, Swann JR, Costabile A, Childs CE, Pedersen C, Goldstone AP, Frost GS. 2014. The impact of oligofructose on stimulation of gut hormones, appetite regulation and adiposity. Obesity 22:1430–1438.
- Müller M, Hermes GDA, Emanuel E C, Holst JJ, Zoetendal EG, Smidt H, Troost F, Schaap FG, Damink SO, Jocken JWE, Lenaerts K, Masclee AAM, Blaak EE. 2020. Effect of wheat bran derived prebiotic supplementation on gastrointestinal transit, gut microbiota, and metabolic health: a randomized controlled trial in healthy adults with a slow gut transit. Gut Microbes 12:1704141.
- Freeland KR, Wilson C, Wolever TMS. 2010. Adaptation of colonic fermentation and glucagon-like peptide-1 secretion with increased wheat fibre intake for 1 year in hyperinsulinaemic human subjects. Br J Nutr 103:82–90.
- Holscher HD, Taylor AM, Swanson KS, Novotny JA, Baer DJ. 2018. Almond consumption and processing affects the composition of the gastrointestinal microbiota of healthy adult men and women: a randomized controlled trial. Nutrients 10:126.
- Ren M, Zhang H, Qi J, Hu A, Jiang Q, Hou Y, Feng Q, Ojo O, Wang X. 2020. An almond-based low carbohydrate diet improves depression and glycometabolism in patients with type 2 diabetes through modulating gut microbiota and GLP-1: a randomized controlled trial. Nutrients 12:3036.
- Shen L, Keenan MJ, Raggio A, Williams C, Martin RJ. 2011. Dietary-resistant starch improves maternal glycemic control in goto-kakizaki rat. Mol Nutr Food Res 55:1499–1508.
- Li M, Trapika IGSC, Tang SYS, Cho J-L, Qi Y, Li CG, Li Y, Yao M, Yang D, Liu B, Li R, Yang P, Ma G, Ren P, Huang X, Xie D, Chen S, Li M, Yang L, Leng P, Huang Y, Li GQ. 2021. Mechanisms and active compounds polysaccharides and bibenzyls of medicinal dendrobiums for diabetes management. Front Nutr 8:811870.
- Dao T-MA, Waget A, Klopp P, Serino M, Vachoux C, Pechere L, Drucker DJ, Champion S, Barthélemy S, Barra Y, Burcelin R, Sérée E. 2011. Resveratrol increases glucose induced GLP-1 secretion in mice: a mechanism which contributes to the glycemic control. PLoS One 6:e20700.
- Yuan T, Yin Z, Yan Z, Hao Q, Zeng J, Li L, Zhao J. 2020. tetrahydrocurcumin ameliorates diabetes profiles of db/db mice by altering the composition of gut microbiota and up-regulating the expression of GLP-1 in the pancreas. Fitoterapia 146:104665.
- Li X-X, Zhang X-X, Zhang R, Ni Z-J, Elam E, Thakur K, Cespedes-Acuña CL, Zhang J-G, Wei Z-J. 2021. Gut modulation based anti-diabetic effects of carboxymethylated wheat bran dietary fiber in high-fat diet/streptozotocin-induced diabetic mice and their potential mechanisms. Food Chem Toxicol 152:112235.
- Yang T, Zhou W, Xu W, Ran L, Yan Y, Lu L, Mi J, Zeng X, Cao Y. 2022. Modulation of gut microbiota and hypoglycemic/hypolipidemic activity of flavonoids from the fruits of Lycium barbarum on high-fat diet/streptozotocin-induced type 2 diabetic mice. Food Funct 13:11169– 11184.
- Chen LC, Fan ZY, Wang HY, Wen DC, Zhang SY. 2019. Effect of polysaccharides from adlay seed on anti-diabetic and gut microbiota. Food Funct 10:4372–4380.
- Koopen A, Witjes J, Wortelboer K, Majait S, Prodan A, Levin E, Herrema H, Winkelmeijer M, Aalvink S, Bergman J, et al. 2022. Duodenal Anaerobutyricum soehngenii infusion stimulates GLP-1 production, ameliorates glycaemic control and beneficially shapes the duodenal transcriptome in metabolic syndrome subjects: a randomised double-blind placebo-controlled cross-over study. Gut 71:1577–1587.
- Simon M-C, Strassburger K, Nowotny B, Kolb H, Nowotny P, Burkart V, Zivehe F, Hwang J-H, Stehle P, Pacini G, Hartmann B, Holst JJ, MacKenzie C, Bindels LB, Martinez I, Walter J, Henrich B, Schloot NC, Roden M. 2015. Intake of Lactobacillus reuteri improves incretin and insulin secretion in glucose-tolerant humans: a proof of concept. Diab Care 38:1827–1834
- Alisi A, Bedogni G, Baviera G, Giorgio V, Porro E, Paris C, Giammaria P, Reali L, Anania F, Nobili V. 2014. Randomised clinical trial: the beneficial effects of VSL#3 in obese children with non-alcoholic steatohepatitis. Aliment Pharmacol Ther 39:1276–1285.
- Xu S, Wang Y, Wang J, Geng W. 2022. Kombucha reduces hyperglycemia in type 2 diabetes of mice by regulating gut microbiota and its metabolites. Foods 11:754.
- Chen YC, Huang SD, Tu JH, Yu JS, Nurlatifah AO, Chiu WC, Su YH, Chang HL, Putri DA, Cheng HL. 2020. Exopolysaccharides of bacillus amyloliquefaciens modulate glycemic level in mice and promote glucose uptake of cells through the activation of AKT. Int J Biol Macromol 146:202–211.
- Yadav H, Lee JH, Lloyd J, Walter P, Rane SG. 2013. Beneficial metabolic effects of a probiotic via butyrate-induced GLP-1 hormone secretion. J Biol Chem 288:25088–25097.
- Ryan PM, Patterson E, Kent RM, Stack H, O’Connor PM, Murphy K, Peterson VL, Mandal R, Wishart DS, Dinan TG, Cryan JF, Seeley RJ, Stanton C, Ross RP. 2017. Recombinant incretin-secreting microbe improves metabolic dysfunction in high-fat diet fed rodents. Sci Rep 7:13523.
- Wang Y, Dilidaxi D, Wu Y, Sailike J, Sun X, Nabi X-H. 2020. Composite probiotics alleviate type 2 diabetes by regulating intestinal microbiota and inducing GLP-1 secretion in db/db mice. Biomed Pharmacother 125:109914.
- Li X, Wang E, Yin B, Fang D, Chen P, Wang G, Zhao J, Zhang H, Chen W. 2017. Effects of Lactobacillus casei CCFM419 on insulin resistance and gut microbiota in type 2 diabetic mice. Benef Microbes 8:421–432.
- Jia L, Li D, Feng N, Shamoon M, Sun Z, Ding L, Zhang H, Chen W, Sun J, Chen YQ. 2017. Anti-diabetic effects of Clostridium butyricum CGMCC0313.1 through promoting the growth of gut butyrate-producing bacteria in type 2 diabetic mice. Sci Rep 7:7046.
- Archer AC, Muthukumar SP, Halami PM. 2021. Lactobacillus fermentum MCC2759 and MCC2760 alleviate inflammation and intestinal function in high-fat diet-fed and streptozotocin-induced diabetic rats. Probiotics Antimicrob Proteins 13:1068–1080.
- Palani Kumar MK, Halami PM, Serva Peddha M. 2021. Effect of Lactobacillus fermentum MCC2760-based probiotic curd on hypercholesterolemic C57Bl6 mice. ACS Omega 6:7701– 7710.
- Singh S, Sharma RK, Malhotra S, Pothuraju R, Shandilya UK. 2017. Lactobacillus Rhamnosus NCDC17 ameliorates type-2 diabetes by improving gut function, oxidative stress and inflammation in high-fat-diet fed and streptozotocintreated rats. Benef Microbes 8:243– 255.
- Lin S, Yang X, Long Y, Zhong H, Wang P, Yuan P, Zhang X, Che L, Feng B, Li J, Zhuo Y, Lin Y, Xu S, Wu D, Fang Z. 2020. Dietary supplementation with Lactobacillus plantarum modified gut microbiota, bile acid profile and glucose homoeostasis in weaning piglets. Br J Nutr 124:797– 808.
- Grasset E, Puel A, Charpentier J, Collet X, Christensen JE, Tercé F, Burcelin R. 2017. A specific gut microbiota Dysbiosis of type 2 diabetic mice induces GLP-1 resistance through an Enteric NO-dependent and gut-brain axis mechanism. Cell Metab 26:278.
- Zhang X, Ren H, Zhao C, Shi Z, Qiu L, Yang F, Zhou X, Han X, Wu K, Zhong H, Li Y, Li J, Ji L. 2022. Metagenomic analysis reveals Crosstalk between gut microbiota and glucose-lowering drugs targeting the gastrointestinal tract in chinese patients with type 2 diabetes: a 6 month, two-arm randomised trial. Diabetologia 65:1613–1626.
- Pulimeno P, Mannic T, Sage D, Giovannoni L, Salmon P, Lemeille S, Giry-Laterriere M, Unser M, Bosco D, Bauer C, Morf J, Halban P, Philippe J, Dibner C. 2013. Autonomous and self-sustained circadian oscillators displayed in human islet cells. Diabetologia 56:497–507.
- Marcheva B, Ramsey KM, Buhr ED, Kobayashi Y, Su H, Ko CH, Ivanova G, Omura C, Mo S, Vitaterna MH, Lopez JP, Philipson LH, Bradfield CA, Crosby SD, JeBailey L, Wang X, Takahashi JS, Bass J. 2010. Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 466:627–631.
- Lindgren O, Mari A, Deacon CF, Carr RD, Winzell MS, Vikman J, Ahrén B. 2009. Differential islet and incretin hormone responses in morning versus afternoon after standardized meal in healthy men. J Clin Endocrinol Metab 94:2887–2892.
- Martchenko SE, Martchenko A, Cox BJ, Naismith K, Waller A, Gurges P, Sweeney ME, Philpott DJ, Brubaker PL. 2020. Circadian GLP-1 secretion in mice is dependent on the intestinal microbiome for maintenance of diurnal metabolic homeostasis. Diabetes 69:2589– 2602.
- Martchenko SE, Martchenko A, Biancolin AD, Waller A, Brubaker PL. 2021. L-cell arntl is required for rhythmic glucagon-like peptide-1 secretion and maintenance of intestinal homeostasis. Mol Metab 54:101340.
- Biancolin AD, Martchenko A, Mitova E, Gurges P, Michalchyshyn E, Chalmers JA, Doria A, Mychaleckyj JC, Adriaenssens AE, Reimann F, Gribble FM, Gil-Lozano M, Cox BJ, Brubaker PL. 2020. The core clock gene, Bmal1, and its downstream target, the SNARE regulatory protein secretagogin, are necessary for circadian secretion of glucagon-like peptide-1. Mol Metab 31:124–137.
- Zhang Q, Xiao X, Zheng J, Li M, Yu M, Ping F, Wang T, Wang X. 2018. Featured article: structure moderation of gut microbiota in liraglutide-treated diabetic male rats. Exp Biol Med (Maywood) 243:34–44.
- Moreira GV, Azevedo FF, Ribeiro LM, Santos A, Guadagnini D, Gama P, Liberti EA, Saad M, Carvalho C. 2018. Liraglutide modulates gut microbiota and reduces NAFLD in obese mice. J Nutr Biochem 62:143–154.
- Wang H, Wang L, Li Y, Luo S, Ye J, Lu Z, Li X, Lu H. 2021. The HIF-2α/PPARα pathway is essential for liraglutide-alleviated, lipid-induced hepatic steatosis. Biomed Pharmacother 140:111778.
- Liu Q, Cai BY, Zhu LX, Xin X, Wang X, An ZM, Li S, Hu YY, Feng Q. 2020. Liraglutide modulates gut microbiome and attenuates nonalcoholic fatty liver in db/db mice. Life Sci 261:118457.
- Ying X, Rongjiong Z, Kahaer M, Chunhui J, Wulasihan M. 2023. Therapeutic efficacy of liraglutide versus metformin in modulating the gut microbiota for treating type 2 diabetes mellitus complicated with nonalcoholic fatty liver disease. Front Microbiol 14:1088187.
- Smits MM, Fluitman KS, Herrema H, Davids M, Kramer MHH, Groen AK, Belzer C, de Vos WM, Cahen DL, Nieuwdorp M, van Raalte DH. 2021. Liraglutide and sitagliptin have no effect on intestinal microbiota composition: a 12-week randomized placebo-controlled trial in adults with type 2 diabetes. Diabetes Metab 47:101223.
- Rizza S, Pietrucci D, Longo S, Menghini R, Teofani A, Piciucchi G, Montagna M, Federici M. 2023. Impact of insulin Degludec/Liraglutide fixed combination on the gut microbiomes of elderly patients with type 2 diabetes: results from A Subanalysis of A small non-randomised single arm study. Aging Dis 14:319–324.
- Silva-Veiga FM, Miranda CS, Vasques-Monteiro IML, Souza-Tavares H, Martins FF, Daleprane JB, Souza-Mello V. 2022. Peroxisome proliferator-activated receptor-alpha activation and dipeptidyl peptidase-4 inhibition target dysbiosis to treat fatty liver in obese mice. World J Gastroenterol 28:1814–1829.
- Liao X, Song L, Zeng B, Liu B, Qiu Y, Qu H, Zheng Y, Long M, Zhou H, Wang Y, Du Y, Xu J, Shen R, Tong Q, Cai L, Li X, Guo S, Yang G, Zhu Z, Pu X, Wei H, Zheng H. 2019. Alteration of gut microbiota induced by DPP-4I treatment improves glucose homeostasis. EBioMedicine 44:665–674.
- Olivares M, Neyrinck AM, Pötgens SA, Beaumont M, Salazar N, Cani PD, Bindels LB, Delzenne NM. 2018. The DPP-4 inhibitor vildagliptin impacts the gut microbiota and prevents disruption of intestinal homeostasis induced by a Western diet in mice. Diabetologia 61:1838– 1848.
- Zhang M, Feng R, Yang M, Qian C, Wang Z, Liu W, Ma J. 2019. Effects of metformin, acarbose, and sitagliptin monotherapy on gut microbiota in zucker diabetic fatty rats. BMJ Open Diabetes Res Care 7:e000717.
- Ryan PM, Patterson E, Carafa I, Mandal R, Wishart DS, Dinan TG, Cryan JF, Tuohy KM, Stanton C, Ross RP. 2020. Metformin and dipeptidyl peptidase-4 inhibitor differentially modulate the intestinal microbiota and plasma metabolome of metabolically dysfunctional mice. Can J Diabetes 44:146–155.
- Zhang Q, Xiao X, Li M, Yu M, Ping F, Zheng J, Wang T, Wang X, Peterson JM. 2017. Vildagliptin increases butyrate-producing bacteria in the gut of diabetic rats. PLoS ONE 12:e0184735.
- Guo S, Al-Sadi R, Said HM, Ma TY. 2013. Lipopolysaccharide causes an increase in intestinal tight junction permeability in vitro and in vivo by inducing enterocyte membrane expression and localization of TLR-4 and CD14. Am J Pathol 182:375–387.
- Zhou S-Y, Gillilland M III, Wu X, Leelasinjaroen P, Zhang G, Zhou H, Ye B, Lu Y, Owyang C. 2018. FODMAP diet modulates visceral nociception by lipopolysaccharide-mediated intestinal inflammation and barrier dysfunction. J Clin Invest 128:267–280.
- Chen Q, Ma X, Li C, Shen Y, Zhu W, Zhang Y, Guo X, Zhou J, Liu C. 2020. Enteric phageome alterations in patients with type 2 diabetes. Front Cell Infect Microbiol 10:575084.
- Ellingsgaard H, Hauselmann I, Schuler B, Habib AM, Baggio LL, Meier DT, Eppler E, Bouzakri K, Wueest S, Muller YD, Hansen AMK, Reinecke M, Konrad D, Gassmann M, Reimann F, Halban PA, Gromada J, Drucker DJ, Gribble FM, Ehses JA, Donath MY. 2011. Interleukin-6 enhances insulin secretion by increasing glucagon-like peptide-1 secretion from L cells and alpha cells. Nat Med 17:1481–1489.
- Costa A, Ai M, Nunn N, Culotta I, Hunter J, Boudjadja MB, Valencia-Torres L, Aviello G, Hodson DJ, Snider BM, Coskun T, Emmerson PJ, Luckman SM, D’Agostino G. 2022. Anorectic and aversive effects of GLP-1 receptor agonism are mediated by brainstem cholecystokinin neurons, and modulated by GIP receptor activation. Mol Metab 55:101407.
- Yusta B, Baggio LL, Koehler J, Holland D, Cao X, Pinnell LJ, Johnson-Henry KC, Yeung W, Surette MG, Bang KWA, Sherman PM, Drucker DJ. 2015. GLP-1R agonists modulate enteric immune responses through the intestinal intraepithelial lymphocyte GLP-1R. Diabetes 64:2537–2549.
- Sharon G, Cruz NJ, Kang DW, Gandal MJ, Wang B, Kim YM, Zink EM, Casey CP, Taylor BC, Lane CJ, Bramer LM, Isern NG, Hoyt DW, Noecker C, Sweredoski MJ, Moradian A, Borenstein E, Jansson JK, Knight R, Metz TO, Lois C, Geschwind DH, Krajmalnik-Brown R, Mazmanian SK. 2019. Human gut microbiota from autism spectrum disorder promote behavioral symptoms in mice. Cell 177:1600–1618.
- Breton J, Tirelle P, Hasanat S, Pernot A, L’Huillier C, do Rego J-C, Déchelotte P, Coëffier M, Bindels LB, Ribet D. 2021. Gut microbiota alteration in a mouse model of anorexia nervosa. Clin Nutr 40:181–189.
- Ren HX, Tang QC, Yan L, Xia H, Luo HS. 2018. Evodiamine inhibits gastrointestinal motility via CCK and CCK1 receptor in water-avoidence stress rat model. Life Sci 209:210–216.
- Marra A, Hanson MA, Kondo S, Erkosar B, Lemaitre B, Ja WW, McFall-Ngai MJ. 2021. Drosophila antimicrobial peptides and lysozymes regulate gut microbiota composition and abundance. mBio 12:e0082421.
- Li Z, Zhang B, Wang N, Zuo Z, Wei H, Zhao F. 2023. A novel peptide protects against diet-induced obesity by suppressing appetite and modulating the gut microbiota. Gut 72:686–698.




